
by Katelyn O’Brien, PharmD, BCPS, CDCES, BC-ADM
The holy month of Ramadan falls on the ninth month of the lunar calendar. In 2023, Ramadan will begin at sundown on March 22nd and end April 20th. Ramadan involves fasting every day for one month, between dawn and sunset. Fasting is an important component of Ramadan for Muslims, demonstrating devotion to the Islamic faith. Fasting is not recommended for everyone. People who are ill or live with high-risk medical conditions, including some people with diabetes (PWD), are exempt. However, a majority of PWD choose to fast. Pharmacists can play a vital role in helping patients to safely participate and provide PWD recommendations on the timing of medications or dosing adjustments to minimize hypoglycemia risks. It can be useful to consult the IDF-DAR Diabetes and Ramadan Practical Guidelines when managing PWD who fast during Ramadan. These guidelines are a practical tool to help healthcare providers support their patients who wish to fast.
Fasting During Ramadan
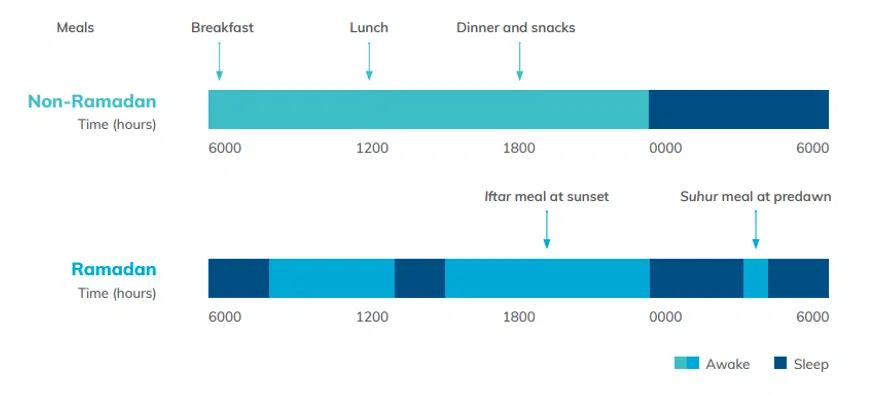
Understanding the fast: Suhoor is the pre-dawn meal and Iftar is the sunset meal which “breaks the fast.” Ifar is usually a bigger meal containing sugar and carbohydrates. The Ramadan Nutrition Plan (RNP) for individuals with diabetes recommends consuming adequate calories with balanced proportions of macronutrients during non-fasting periods to prevent hypoglycemia during the fasting period. PWD should be educated to equally distribute carbohydrate intake between meals to minimize post-prandial hyperglycemia. Many patients will have fragmented sleep patterns during Ramadan and these changes in sleep patterns can also affect glucose levels.
When to break the fast: If glucose drops <70 mg/dL or if there are symptoms of hypoglycemia, the PWD should break the fast and treat hypoglycemia with fast acting carbohydrate such as 4 oz of juice, milk, or sugary beverage and recheck glucose in 15 minutes. If glucose is >300 mg/dL or if the patient is experiencing symptoms of hyperglycemia, dehydration, or acute illness, the fast should also be broken to prevent AKI and/or DKA.
Medication Management
Metformin does not cause hypoglycemia, and therefore is considered safe to continue during Ramadan, but consider adjusting the timing of doses to minimize GI upset.
| Once daily IR or ER dosing | Twice daily dosing | Three times daily dosing |
| No dose modification required | No dose modification required | Morning dose to be taken before suhoor |
| Take at iftar | Take at iftar and suhoor | Combine afternoon dose with dose to be taken after iftar |
Sulfonylureas (SUs) stimulate insulin secretion from the beta cells in the pancreas, independent of blood glucose, and therefore PWD taking this medication are at higher risk for hypoglycemia while fasting.
| Once daily dosing | Twice daily dosing |
| Take at iftar | Iftar dose remains the same |
| If diabetes is well controlled, consider dose reduction to avoid hypoglycemia | If diabetes is well controlled, reduce dose with Suhoor |
Thiazolidinediones (TZDs) improve insulin sensitivity of the fat, muscle, liver and peripheral tissues. TZDs work without increasing insulin secretion, the risk of hypoglycemia when used as monotherapy is very low. No dose modifications are needed during fasting; it should be taken with iftar.
Sodium-glucose co-transporter 2 inhibitors (SGLT2i) work to reduce glucose levels by increasing urinary excretion of glucose. When taken as monotherapy, this class of medication has little to no risk for hypoglycemia and therefore is a safe treatment choice for individuals who chose to fast during Ramadan. However, there are safety concerns due dehydration and the risks for euglycemic DKA. No dose adjustments are required during Ramadan. Based on data from trials studying SGLT2i use during Ramadan, some experts recommend holding off starting patients on a SGLT2i in the 4 weeks leading up to Ramadan. PWD should increase fluid intake while having iftar and suhoor to ensure adequate hydration. Take the SGLT2i with iftar meal.
Dipeptidyl peptidase-4 inhibitors (DPP-4i) block the DPP-4 enzyme and thereby increase the amount of GLP1 circulating to stimulate insulin secretion. These medications have a low risk for hypoglycemia. There have been several randomized controlled trials looking at the effects from switching to DPP4, overall the risk of hypoglycemia decreased in DPP4 compared with SU. No dosage adjustments are needed.
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) mimic the incretin hormone and reduces glucose by increasing insulin release in a glucose dependent manner. Since they act in a glucose dependent manner, this class of medications has a lower risk for hypoglycemia when used as monotherapy. Studies have been done with liraglutide, exenatide, and lixisenatide during Ramadan and all are deemed safe to use with a low risk for hypoglycemia. Provided that the GLP-1 RAs have been appropriately dose titrated at least 2-4 weeks prior to Ramadan, no modifications in therapy are needed.
Insulin dose adjustments may be required before Ramadan to prevent hypoglycemia and during Ramadan if hypoglycemia occurs. Consider using longer acting basal insulins having lower hypoglycemia risks than NPH.
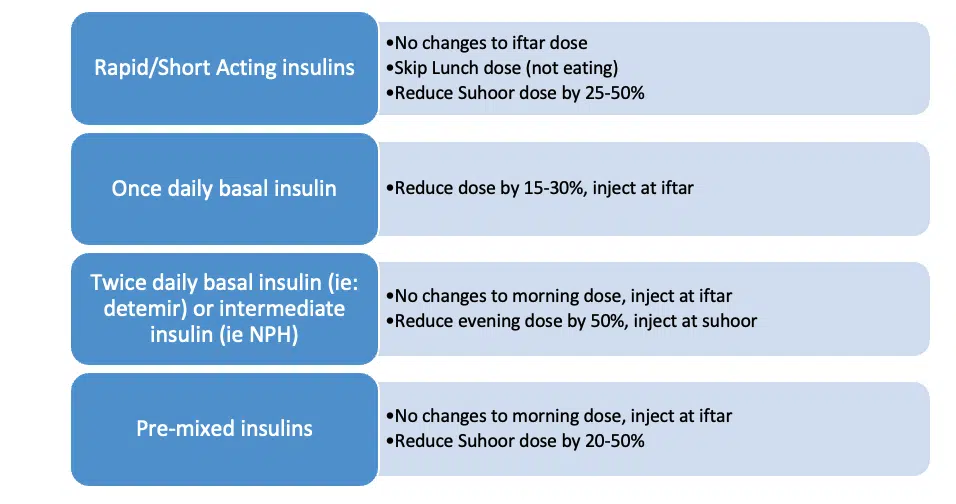
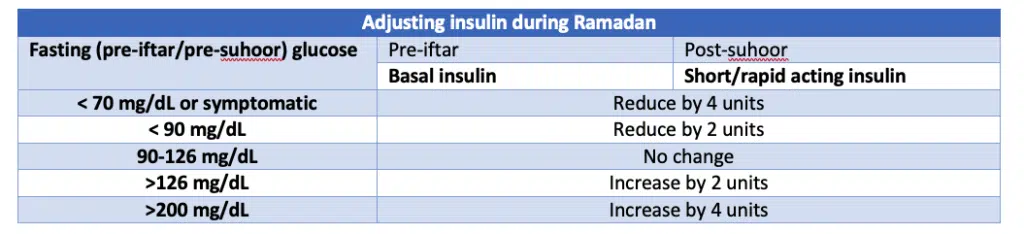
See the IDF and DAR International Alliance guidelines for additional recommendations on adjusting basal and bolus insulins.
Monitoring Glucose
PWD should be given specific instructions when to monitor their blood glucose. At a minimum, BG should be checked 1-2 times per day for those with T2DM, preferrably pre-iftar (fasting) and post-suhoor. In patients with T1DM or T2DM on multiple insulin administrations per day, experts recommend measuring glucose levels several times per day. Continuous glucose monitors can be useful if hypoglycemia is a major concern and can alert PWD to hypoglycemia or hyperglycemia.
References International Diabetes Federation and DAR International Alliance. Diabetes and Ramadan: Practical Guidelines, Brussels, Belgium: International Diabetes Federation, 2021. Sheikh A, Das B, Sattar S. et al. Safety of sodium-glucose cotransporter 2 inhibitors (SGLT2i) during the month of Ramadan in patients with type 2 diabetes mellitus in Pakistani population—an observational study from a tertiary care center in Karachi. Endocrine 2022 Dec 29;1-7. doi: 10.1007/s12020-022-03290-7.




 iForumRx.org is a web-based community of practice designed to inform ambulatory care pharmacy specialists, pharmacy residents, and student pharmacists about high-quality, practice-changing evidence.
iForumRx.org is a web-based community of practice designed to inform ambulatory care pharmacy specialists, pharmacy residents, and student pharmacists about high-quality, practice-changing evidence.
Great article. Thank you for this information!