by Jessica L Lucido, Doctor of Pharmacy Candidate, University of Mississippi School of Pharmacy
Asthma is one of the most common chronic diseases that affected an estimated 262 million people worldwide in 2019. Unfortunately, asthma is frequently undiagnosed and undertreated, thus asthma-related morbidity and mortality remain significant.1,2 The Global Initiative for Asthma (GINA) provides evidence based recommendations for the management and prevention of asthma. GINA is a valuable resource for healthcare providers, and continues to provide up-to-date information on asthma care and prevention. In 2002, the GINA Science Committee was established to perform a twice-yearly review and update of new scientific evidence for asthma management.4 This ongoing review process ensures that the guidelines remain relevant and evidence-based, helping healthcare providers deliver optimal care to asthma patients. The 2024 updates include alternative testing strategies to diagnose asthma, an updated mindset towards treatment, and new recommendations for first line treatment options.4
Alternate Diagnostic Testing Strategies
Spirometry is a very useful tool to assess pulmonary function in patients suspected of having asthma or other pulmonary diseases.5 However, access to spirometry is lacking in many places with limited healthcare resources. The significant underdiagnosis and undertreatment of asthma has led researchers to explore the challenges associated with testing in an effort to improve early detection and treatment outcomes.6 The GINA guidelines reference a recent study that found timely access to spirometry was not feasible in many places due to lack of equipment and trained personnel.5 In response, GINA is now advocating for the use of other pulmonary function tests such as Peak Expiratory Flow (PEF) monitoring when spirometry is not available.4 While PEF monitoring is less reliable than spirometry, it provides more information than relying on symptoms alone and is a more accessible tool.5 The Diagnostic Flowchart (see GINA 2024 Guidelines – Box 1.1) has been updated to reflect a step-by-step approach to asthma assessment including symptoms, patient history, current asthma medication, and lung function test availability.4 Furthermore, the flowchart goes on to recommend empiric treatment of asthma symptoms with inhaled corticosteroid (ICS)-containing treatments in the absence of a lung functions test.4 By incorporating the use of alternative diagnostic tools and empiric ICS-containing treatment, this update aims to reduce morbidity and mortality in settings where traditional diagnostic methods are not readily available.5
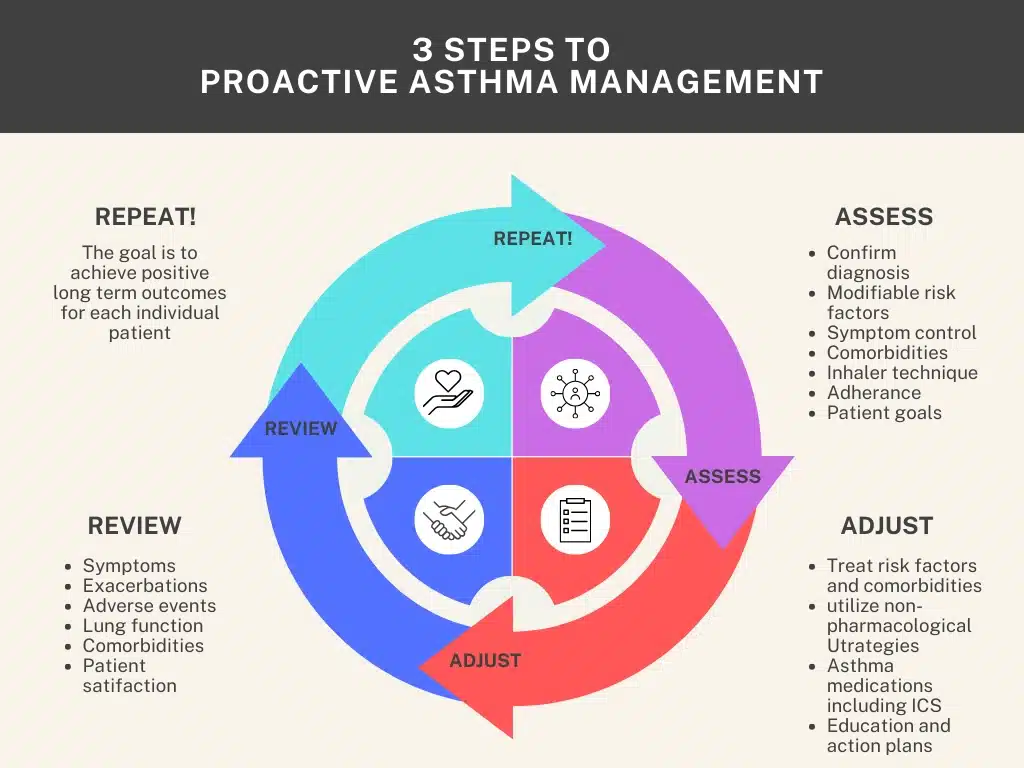
Continuous Care and Proactive Management
Asthma is often viewed and treated as a recurrent acute disease whereby treatment fluctuates based on the patient’s symptoms rather than focusing on long-term management.4 Even patients with few symptoms can have severe exacerbations leading to poor outcomes.7 These inconsistencies in care can lead to increased morbidity and mortality and require a change in asthma management.8 A study referenced by the updated GINA guidelines states “Successful management depends on promoting adherence of both healthcare providers and patients to treatment,” emphasizing the role healthcare providers have in ensuring continuity and long-term adherence to treatment plans.8 Recognizing asthma as a chronic illness is the first step in embracing a shift towards continuous care and proactive management. The new asthma management cycle focuses on three main steps: Assess, Adjust, and Review.4 Each step encourages practitioners to evaluate not only symptoms but also comorbidities, risk factors, adherence, patient knowledge, and patient goals.4 Adopting this comprehensive management approach addresses the multifaceted nature of asthma and aligns with the principles of managing chronic disease states.8 The GINA cycle of asthma management aims to emphasize personalized asthma treatment in an effort to improve long-term patient outcomes.4
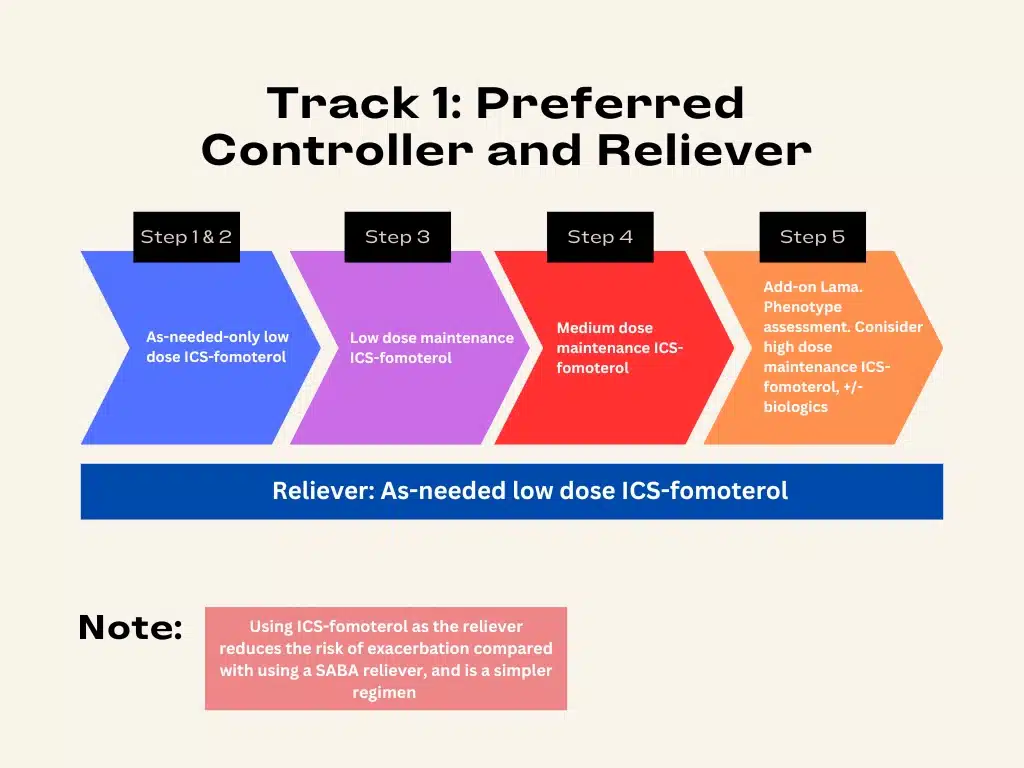
Recommended First-Line Treatments
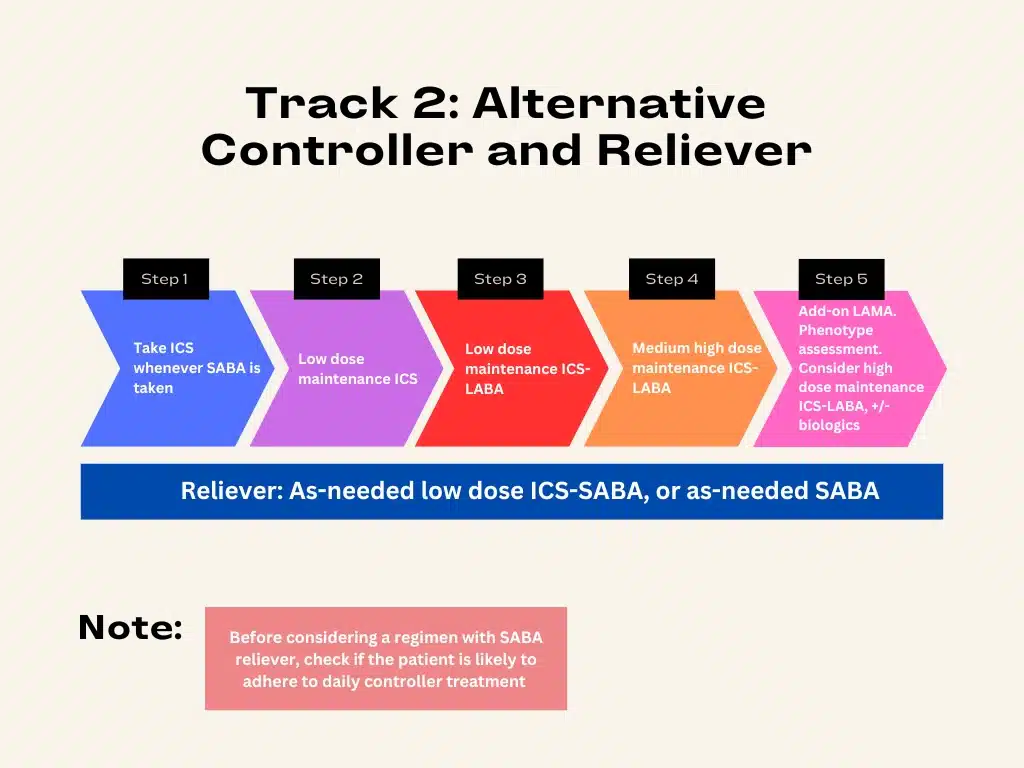
The GINA guidelines now recommend the use of inhaled corticosteroid-containing medications as maintenance and reliever therapy.4 GINA has recommended against the use of regular SABA-only therapy since 2019 due to increased airway hyperresponsiveness, diminished bronchodilator effect, and increased eosinophilia.4 Moreover, SABA therapy trains patients to perceive it as their primary form of treatment, which results in poor adherence to ICS therapy.4 One study compared the use of as-needed SABA-only therapy, terbutaline, to as-needed use of ICS-formoterol with terbutaline.9 As needed ICS-formoterol in combination with terbutaline had a 64% reduction in the rate of severe exacerbations and 60% reduction in moderate to severe exacerbation when compared with terbutaline alone.9 Another study comparing as-needed budesonide-formoterol with as-needed albuterol, the SABA reliever therapy most often prescribed in North America, resulted in significantly lower exacerbation rate and fewer severe exacerbations.10 This evidence strongly supports the shift in recommendations from SABA-only therapy to using ICS-containing combinations for both reliever and maintenance therapy.10 This change is reflected in Track 1 where steps 1 and 2 recommend as-needed ICS-formoterol, step 3 recommends low-dose ICS-formoterol as maintenance therapy plus as-needed use, and step 4 escalates to moderate-dose ICS-formoterol with as-needed use.11 Step 5 still recommends the use of additional therapies such as LAMAs and biologics.11 The aim of these recommendations are to improve asthma control while simplifying medication regimens.
The GINA guidelines also provide alternatives for asthma management in Track 2, which now recommends the use of as needed ICS therapy in addition to as needed SABA.4 This recommendation is supported by a study that investigated whether the as needed use of salbutamol was noninferior to regular use of beclomethasone and superior to as needed use of albuterol.12 They found that as needed ICS-SABA therapy was as effective as regular ICS therapy for asthma control and is superior to using as needed SABA-only therapy.12 This evidence supports a more flexible approach to asthma control for patients who struggle with daily adherence to their medications.4 It also encourages the use of anti-inflammatory therapy, which is key for reducing long-term asthma complications and improving overall disease control.12 Thus an ICS should be used whenever SABA is used for symptom control.4 Step 2 recommends using low dose ICS as maintenance and as needed ICS-SABA, but patient adherence should be assessed when transitioning patients from step 1 to step 2 to prevent SABA-only use.4 These changes offer a more adaptable and patient-centered approach to asthma management promoting effective symptom control and improving long-term outcomes.
The 2024 GINA updates shift asthma management from reactive to proactive. The guidelines promote early intervention, focus on continuous care, and aim to reduce severe exacerbations. While the guidelines continue to endorse spirometry as one of the most reliable diagnostic tests for asthma, they now encourage the use of PEF to improve earlier detection and diagnosis. Changing the view of asthma management from acute to continuous care allows providers to take a more holistic approach that is consistent with other chronic diseases with an aim of improving long-term outcomes. The addition of ICS-containing inhalers as both reliever and maintenance therapy emphasizes the need for long-term control and simplification of treatment regimens. The GINA 2024 updates provide many resources and recommendations that empower healthcare providers to offer more personalized, accessible, and effective care to their patients.
References
- World Health Organization: Asthma [Internet]. 6 May 2024. [cited 2024 Jan 27] Available from” https://www.who.int/news-room/fact-sheets/detail/asthma
- Asthma: FastStats. CDC: National Center for Health Statistics. [Internet] 31 July 2024 [cited 2024 Jan 27]. Available from: https://www.cdc.gov/nchs/fastats/asthma.htm
- Global Initiative for Asthma – GINA. About US – Global Initiative for Asthma [Internet]. Global Initiative for Asthma – GINA. 2024. [cited 2024 Jan 27] Available from: https://ginasthma.org/
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2024. Updated May 2024. [cited 2024 Jan 27] Available from: https://ginasthma.org/2024-report/
- Mortimer K, Masekela R, Ozoh OB, et al. The reality of managing asthma in sub-Saharan Africa – Priorities and strategies for improving care. J Pan Afr Thorac Soc 2022;3:105-20.
- Haahtela T, Tuomisto LE, Pietinalho A, et al. A 10 year asthma programme in Finland: major change for the better. Thorax. 2006 Aug;61(8):663-70. doi: 10.1136/thx.2005.055699.
- Dusser D, Montani D, Chanez P, et al. Mild asthma: an expert review on epidemiology, clinical characteristics and treatment recommendations. Allergy 2007; 62: 591-604. https://doi.org/10.1111/j.1398-9995.2007.01394.x
- Saglani S, Menzie-Gow AN. Approaches to Asthma Diagnosis in Children and Adults. Front Pediatr 2019 Apr 17;7:148. doi: 10.3389/fped.2019.00148.
- O’Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled Combined Budesonide-Formoterol as Needed in Mild Asthma. N Engl J Med 2018;378(20):1865-1876. doi: 10.1056/NEJMoa1715274.
- Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, Harrison T, Houghton C, Oldfield K, Papi A, Pavord ID, Williams M, Weatherall M. Controlled trial of Budesonide–Formoterol as needed for mild asthma. N Eng J Med 2019;380(21):2020–2030.
- Dubin S, Patak P, Jung D. Update on Asthma Management Guidelines. Mo Med. 2024 Sep-Oct;121(5):364-367. PMID: 39421468; PMCID: PMC11482852
- Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, Crimi N, Vignola AM, Morelli P, Nicolini G, Fabbri LM. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. N Eng J Med 2007;356(20):2040–2052.


 iForumRx.org is a web-based community of practice designed to inform ambulatory care pharmacy specialists, pharmacy residents, and student pharmacists about high-quality, practice-changing evidence.
iForumRx.org is a web-based community of practice designed to inform ambulatory care pharmacy specialists, pharmacy residents, and student pharmacists about high-quality, practice-changing evidence.